The European Union (EU) has been supporting the global fight against COVID-19 since the start of the pandemic, and it is committed to making national health systems more resilient. Partner countries have faced many challenges including the distribution of emergency supplies to strengthen local health systems, the launch of national vaccination campaigns and the boosting of economic recovery. The EU has supported its partners across the world wherever necessary and whenever possible, including in Zimbabwe.
Under Team Europe, the EU global response to the COVID-19 pandemic has amounted to €46 billion. Many other initiatives have been taken in partnership with, or exclusively by, the EU such as the Coronavirus Global Response, the access to COVID-19 Tools (ACT) Accelerator, COVAX and the EU vaccine-sharing mechanism.
The EU-funded Universal Health Coverage Partnership (which covers 115 countries and areas including Zimbabwe) helps deliver World Health Organisation (WHO) support and technical expertise in advancing Universal Health Coverage (UHC)1 with a primary health care approach.2
The Universal Health Coverage Partnership in Zimbabwe
The COVID-19 pandemic has left many people in Zimbabwe unable to visit health clinics due to prevention and containment measures, national lockdowns and associated fears of contracting the virus.3 This means they have missed out on services such as immunization, reproductive and maternal health, and prevention and treatment of chronic diseases. More than 80% of facilities reported a decline in uptake of essential health services, prompting the Government of Zimbabwe to take action to ensure people could get the services they need, and to step up action to maintain the safety of all frontline health workers and patients.
WHO Zimbabwe, with support from the UHC Partnership, has worked closely with the Ministry of Health and Child Care (MoHCC), and provided technical assistance to strengthen the delivery of essential health services at rural, district and provincial health facilities – both prior to and during the COVID-19 pandemic.
Lessons learnt from the the UHC Partnership in Zimbabwe:
- Empowering healthcare workers to generate and use data in order to make informed decisions and improve access to essential health services
- Implementing a people-centred approach as a key priority
- Preparing and responding to the COVID-19 crisis with an emergency response plan
1. Empowering healthcare workers to generate and use data in order to make informed decisions and improve access to essential health services
In August 2019, prior to the pandemic, WHO Zimbabwe, through the UHC Partnership, worked with the MoHCC to develop a tool for the weekly routine monitoring of health services.4 This was a means to track the continuity of essential health services. WHO Zimbabwe trained MoHCC staff at central, provincial and district hospitals and at primary care facilities on how to use the weekly routine monitoring tool. When the COVID-19 outbreak began, the MoHCC, with support from WHO Zimbabwe, updated and adapted the tool accordingly.

As a result of the routine monitoring tool, the MoHCC was able to receive data that enabled health workers to identify and address the challenges affecting delivery of essential health services. For example, they embarked on integrated outreach and ensured healthcare workers had access to much-needed personal protective equipment (PPE) – according to the findings of the Infection Prevention and Control (IPC) assessment. The routine monitoring of the health services report was used to inform the prioritization of fieldwork on the Rapid Assessment of continuity of essential services, and to triangulate5 the results of the assessment.
“We envisioned having a system that gives us real-time data; a robust weekly routine monitoring system that rides on an existing system, in this instance the District Health Information System, forming part of the weekly disease surveillance report,” said Dr Rugare Kangwende, MoHCC, Director of Monitoring and Evaluation.
2. Implementing a people-centred approach as a key priority
For Zimbabwe – as elsewhere in Africa – the need to continue non-COVID-19 services such as immunization, access to medicines, sexual and reproductive health including treatment of HIV, and diagnosis and treatment of non-communicable diseases (NCDs), is vital.
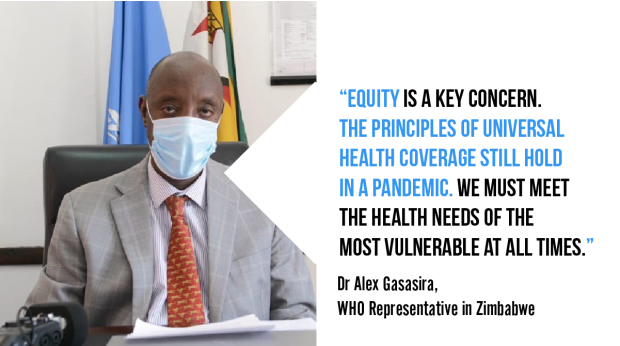
“Equity is a key concern. COVID-19 has the greatest impact on communities that are already vulnerable and marginalized, especially those with high levels of diseases and which have less access to essential health services. The principles of UHC still hold in a pandemic; we must meet the health needs of the most vulnerable at all times,” said Dr Alex Gasasira, WHO Representative in Zimbabwe.
Frontline health workers and patients also need to be protected in times of crisis, but this is no easy task. Providing safe health services during a pandemic requires PPE for health workers, proper entrance screening for COVID-19 and triage systems for patients. However, according to a WHO survey conducted in Zimbabwe, 22% of all health facilities did not have this screening point in place and 25% of facilities lacked an isolation room. Where facilities did have screening points, some were devoid of health workers or had inadequate supplies of PPE.6
3. Preparing and responding to the COVID-19 crisis with an emergency response plan
When COVID-19 arrived in Zimbabwe, the government developed an emergency response and preparedness plan comprising of 8 pillars – one of which was case management and continuity of essential health services. To support Zimbabwe on this front, WHO, through the UHC Partnership, collaborated with a range of Global Health Initiative partners including UNICEF, UNFPA, UN Women and Africa Centres for Disease Control and Prevention.
“To mitigate the impact of COVID-19, the MoHCC – with support from UNICEF, WHO and other partners – have developed and rolled out service continuity guidelines which include integrated outreach services across all ten provinces to complement community-based services offered by village health workers. The integrated outreach activities use the primary healthcare approach to bring services closer to people. It is anticipated that, owing to the scale-up of integrated outreach services (started in September 2020 as a COVID-19 response measure), the essential services indicator coverage will continue to improve to pre-COVID-19 levels,” said Dr Paul Ngwakum, UNICEF Zimbabwe Chief of Health and Nutrition.

In October 2020, with support from the UHC Partnership and other partners, the MoHCC conducted a national rapid assessment of the continuity of essential health services in all 10 provinces of Zimbabwe.7 The assessment found a decline in access to essential health services in all 10 provinces as a result of COVID-19. Overall, 6% of all health facilities were completely closed, and 86% reported a decline in attendance. Reasons for the decline of service use included the general situation of the national lockdown and the spread of misinformation, along with fears of catching COVID-19 at health facilities circulating among community members. Health workers were also afraid of contracting COVID-19, exacerbated by a lack of PPE and information. Inadequate capacity and a failure to provide outreach services to the population also added to the problem.
Life-saving decisions rely on robust and timely data
COVID-19 is a strong reminder that the continuity of essential health services needs to be part of a pandemic response. Protecting the most vulnerable in times of calm or crisis is one of the core principles of UHC, and it relies on equitable and resilient health systems. As the case of Zimbabwe has shown, the empowerment of health workers was crucial in maintaining availability and access to essential health services. Moreover, when people have the right information at the right time it makes all the difference in saving lives, providing treatment and preventing disease. Monitoring and analysis of health systems, followed by practical support, is vital to the decision-making process across the health system.
Click on the play button below to watch our video on the Universal Health Coverage Partnership
Have you been involved in health-related interventions in response to the COVID-19 pandemic and its challenges? What approach was implemented?
Did you meet any challenges, and how did you address them?
Leave your comment below!
Credit: Video © Capacity4dev
1 UHC means that all individuals and communities receive the health services they need without suffering financial hardship. It includes the full spectrum of essential, quality health services, from health promotion to prevention, treatment, rehabilitation, and palliative care across the life course. The delivery of these services requires adequate and competent healthcare workers with optimal skills mix at facility, outreach and community level, and who are equitably distributed, adequately supported and enjoy decent working conditions.
2 The Partnership is also funded by the Grand Duchy of Luxembourg, Irish Aid, the Government of Japan, the French Ministry for Europe and Foreign Affairs, the United Kingdom – Foreign, Commonwealth & Development Office, Belgium, Canada and Germany.
3 Zimbabwe reported its first case of COVID-19 on 20 March 2020. A year later, the country had recorded 36,717 cases and 1,516 deaths as of 23 March 2021.
4 The tool collects information from all primary and secondary health facilities nationwide including data on work attendance by health personnel, patient visits to outpatient and casualty emergency departments, patient admissions to hospitals, major operations, renal dialysis sessions, family planning services, postnatal care, institutional and complicated deliveries and antenatal care attendance. It further collects data on institutional and community deaths, immunization and vitamin A supplements, tracer medicines status and tuberculosis diagnosis. It also finds information on HIV testing and viral load, COVID-19 testing and availability of personal protective equipment (PPE).
5 The term triangulation refers to the practice of using multiple sources of data or multiple approaches to analyzing data to enhance the credibility of a research study.
6 Even before COVID-19, the Zimbabwean health system already faced serious challenges with health workforce shortages, low staff morale and infrastructure in need of upgrading.
7 The assessment sought to identify the state of service delivery in communities and any bottlenecks to effective service provision for both COVID-19 cases and other essential services. It also reached out to provincial and district implementers with technical support to solve the related problems they were experiencing.







Comments
Log in with your EU Login account to post or comment on the platform.